

Multifaceted treatment is required when multiple diseases present themselves simultaneously, especially when their symptoms overlap. This is frequently the case with rosacea and seborrheic dermatitis. A survey on 1,099 rosacea patients conducted by the National Rosacea Society found that 25% were also diagnosed with seborrheic dermatitis.
How to Treat Rosacea and Dermatitis
In this article:
- What are the Treatment Options for Rosacea and Seborrheic Dermatitis?
- Steroid Creams
- Anti-Fungal Creams
- The Mother of All Creams
What are the Treatment Options for Rosacea and Seborrheic Dermatitis?
Treatment options vary depending on the location of seborrheic dermatitis or rosacea flare-ups. For example, rosacea of the scalp treatments will likely include rosacea shampoo. Areas around your eyes will require more sensitive products that do not contain steroids. On the flipside, regular application of hydrocortisone for seborrheic dermatitis is the common nasal seborrheic dermatitis treatment.
Let’s look at some of the broader treatments professionals recommend for rosacea dermatitis.
Steroid Creams

Any search for a rosacea and seborrheic dermatitis treatment will yield topical steroid creams. These hydrocortisone-formulated creams are commonly prescribed by doctors. Unfortunately, these products can lead to the thinning of the skin, an undesirable occurrence for the body’s first line of defense. Usage over longer periods of time can also lead to rosacea-like symptoms, such as redness and irritated skin. Additionally, steroid creams don’t pose as a good rosacea dermatitis treatment for sensitive skin, such as the skin around the eyes, due to the damage they can cause.
Anti-Fungal Creams
There are a variety of anti-fungal creams for rosacea and seborrheic dermatitis out there. Scientific studies have shown that ketoconazole is the most effective of the different anti-fungal agents. Others such as clotrimazole fail to properly keep seborrheic dermatitis under control. However, the strength of ketoconazole can prove troublesome for those with sensitive skin. Note that ketoconazole creams can also have side effects similar to the diseases it’s treating such as itching, dryness, or redness of the treated areas.
The Mother of All Creams
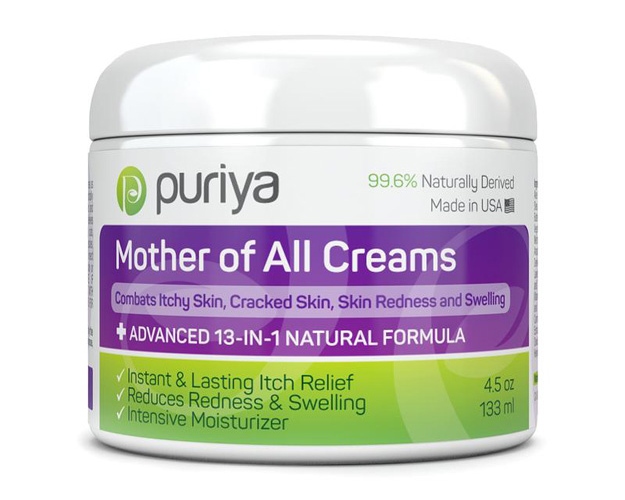
The Mother of All Creams by Puriya is not just a rosacea and dermatitis cream. It’s a topical skincare extravaganza. It can act as a treatment for eczema and rosacea at the same time, eczema and seborrheic dermatitis, and a whole host of other skin issues. Infused with all natural ingredients, you don’t have to worry about the potential dangers of long-term use like you would with topical hydrocortisone steroid creams.
The Mother of All Creams is overflowing with nourishing vitamins that help to heal the skin, all pulled from the arms of mother nature. This unique cream works to hydrate and revitalize the skin with honey, jojoba oil, and MSM. It rejuvenates with the healing aloe vera and carrot seed essential oil. It works to ward off potential allergic reactions with the use of amaranth oil.
Watch this video from Dr. William Groff to find out more about rosacea causes, symptoms, and treatments:
Treating rosacea and dermatitis can be difficult. There are creams for rosacea and dermatitis which pose their own risk of side effects for people with sensitive skin. This makes it important to choose milder and more natural dermatitis and rosacea treatment creams.
What other treatments for rosacea and dermatitis have you tried? What was your experience like? Share them with us in the comments section below!
Up Next: Essential Oil For Psoriasis: Try These 7 Scents
Editor’s Note – This post was originally published on March 20, 2017, and has been updated for quality and relevancy.
